Overview
What is cervical screening?
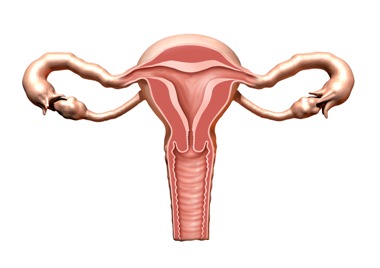
- Cervical screening (a smear test) checks the health of your cervix. The cervix is the opening to your womb from your vagina.
- It's not a test for cancer, it's a test to help prevent cancer.
- All women and people with a cervix aged 25 to 64 should be invited by letter.
- During the screening appointment, a small sample of cells will be taken from your cervix.
- The sample is tested for certain types of human papillomavirus (HPV) that can cause changes to the cells of your cervix. These are called 'high risk' types of HPV.
- If these types of HPV are not found, you do not need any further tests.
- If these types of HPV are found, the sample is then checked for any changes in the cells of your cervix. These can then be treated before they get a chance to turn into cervical cancer.
- You'll get your results by letter, usually in about 2 weeks. It will explain what happens next
Important
Try not to put off cervical screening. It's one of the best ways to protect yourself from cervical cancer.
Why should it be done?
Cervical screening is one of the best ways to protect yourself from cervical cancer.
Cervical screening is not a test for cancer, it's a test to help prevent cancer.
How cervical screening helps prevent cancer
Cervical screening checks a sample of cells from your cervix for certain types of human papillomavirus (HPV).
These types of HPV can cause abnormal changes to the cells in your cervix and are called "high risk" types of HPV.
If these types of HPV are found during screening (an HPV positive result), the sample of cells is then checked for abnormal changes. If abnormal cells are not treated, they may turn into cervical cancer.
What is HPV?
HPV is the name for a very common group of viruses.
Most people will get some type of HPV during their lives. It is very common and nothing to feel ashamed or embarrassed about.
You can get HPV from any kind of skin-to-skin contact of the genital area, not just from penetrative sex.
This includes:
- vaginal, oral or anal sex
- any skin-to-skin contact of the genital area
- sharing sex toys
Some types of HPV (called "high risk" types) can cause cervical cancer. In most cases your body will get rid of HPV without it causing any problems. But sometimes HPV can stay in your body for a long time.
If high risk types of HPV stay in your body, they can cause changes to the cells in your cervix. These changes may become cervical cancer if not treated.
If you do not have a high risk type of HPV it is very unlikely you will get cervical cancer, even if you have had abnormal cell changes in your cervix before.
Find out more about what HPV is
Important
Finding high risk HPV early means you can be monitored for abnormal cell changes.
Abnormal changes can be treated so they do not get a chance to turn into cervical cancer.
Who's at risk of cervical cancer
If you have a cervix and have had any kind of sexual contact, with a man or a woman, you could get cervical cancer. This is because nearly all cervical cancers are caused by infection with high risk types of HPV.
You can get HPV through:
- vaginal, oral or anal sex
- any skin-to-skin contact of the genital area
- sharing sex toys
You're still at risk of cervical cancer if:
- you have had the HPV vaccine – it does not protect you from all types of HPV, so you're still at risk of cervical cancer
- you have only had 1 sexual partner – you can get HPV the first time you're sexually active
- you have had the same partner, or not had sex, for a long time – you can have HPV for a long time without knowing it
- you're a lesbian or bisexual – you're at risk if you have had any sexual contact
- you're a trans man with a cervix
- you have had a partial hysterectomy that did not remove all of your cervix
If you've never had any kind of sexual contact with a man or woman, you may decide not to go for cervical screening when you are invited. But you can still have a test if you want one.
If you're not sure whether to have cervical screening, talk to your GP or nurse.
Cervical screening is a choice
It's your choice if you want to go for cervical screening. But cervical screening is one of the best ways to protect you from cervical cancer.
Risks of cervical screening
You may have some light bleeding or spotting after cervical screening. This should stop within a few hours.
If abnormal cells are found and you need treatment, there are some risks, such as:
- treating cells that may have gone back to normal on their own
- bleeding or an infection
- you may be more likely to have a baby early if you get pregnant in the future – but this is rare
For more information to help you decide, read the NHS cervical screening leaflet.
How to opt out
If you do not want to be invited for screening, contact your GP and ask to be taken off their cervical screening list.
You can ask them to put you back on the list at any time if you change your mind.
When should it be done?
All women and people with a cervix between the ages of 25 and 64 should go for regular cervical screening. You'll get a letter in the post inviting you to make an appointment.
When you'll be invited for cervical screening
From the 1st of January 2022, all women and people with a cervix aged between 25 & 64 will now be recalled for cervical screening every 5 years.
65 or older only if 1 of your last 3 tests was abnormal.
You can book an appointment as soon as you get a letter.
If you missed your last cervical screening, you do not need to wait for a letter to book an appointment.
Visit Public Health Wales for further information on cervical screening.
When cervical screening is not recommended
If you're under 25
You will not be invited for cervical screening until you're 25 because:
- cervical cancer is very rare in people under 25
- it might lead to having treatment you do not need – abnormal cell changes often go back to normal in younger women
If you're 65 or older
You'll usually stop being invited for screening once you turn 65. This is because it's very unlikely that you'll get cervical cancer.
You'll only be invited again if 1 of your last 3 tests was abnormal.
If you're 65 or older and have never been for cervical screening, or have not had cervical screening since the age of 50, you can ask your GP for a test.
If you have had a total hysterectomy
You will not need to go for cervical screening if you have had a total hysterectomy to remove all of your womb and cervix.
You should not receive any more screening invitation letters.
Information for carers and the people they support
Carers and care providers play an essential role in making sure that the people they care for feel supported to access screening when invited. You can find out more about this here.
See a GP if:
You're worried about symptoms of cervical cancer such as:
- bleeding between periods, during or after sex, or after you have been through the menopause
- unusual vaginal discharge
Do not wait for your next cervical screening appointment.
How to book
You'll be sent an invitation letter in the post when it's time to book your cervical screening appointment.
Your letter will tell you where you can go for cervical screening and how to book.
Most cervical screening is done in a GP surgery by a female nurse or doctor.
Call your GP surgery to book an appointment with them. You might be able to book the appointment online.
If you missed an appointment
If you were invited for cervical screening but missed or did not book an appointment, you can contact your GP surgery to book now.
You can still book even if you were invited weeks or months ago.
When to book cervical screening
Try to book your appointment as soon as you get invited. If you missed your last cervical screening, you do not need to wait for a letter.
It's best to book an appointment when:
- you're not having a period – also try to avoid the 2 days before or after you bleed (if you do not have periods, you can book any time)
- you have finished treatment if you have unusual vaginal discharge or a pelvic infection
Important
Avoid using any vaginal medications, lubricants or creams in the 2 days before you have your test as they can affect the results.
Things to ask when you book
It's OK to let the GP surgery know if you have any worries about going for cervical screening.
Do:
- let them know if you'd like a woman to do the test – most nurses and doctors who take cervical screening samples are female
- let them know if you'd like someone else to be in the room with you (a chaperone) – this could be someone you know, another nurse or a trained member of staff
- ask for a longer appointment if you think you might need more time – some GPs can offer a double booking
- let them know if you're finding the test more difficult after going through the menopause – they can prescribe a vaginal oestrogen cream or pessary before the test
- ask for a smaller speculum (a smooth, tube-shaped tool that's put into your vagina so they can see your cervix)
Don't:
- try not to be embarrassed about talking to the nurse or doctor on the day – they're trained to make you feel more comfortable and provide support
How is it performed?
During cervical screening a small sample of cells is taken from your cervix for testing.
The test itself should take less than 5 minutes. The whole appointment should take about 10 minutes.
It's usually done by a female nurse or doctor.
Before starting, they should explain what will happen during the test and answer any questions you have.
How cervical screening is done
- You'll need to undress, behind a screen, from the waist down. You'll be given a sheet to put over you.
- The nurse will ask you to lie back on a bed, usually with your legs bent, feet together and knees apart. Sometimes you may need to change position during the test.
- They'll gently put a smooth, tube-shaped tool (a speculum) into your vagina. A small amount of lubricant may be used.
- The nurse will open the speculum so they can see your cervix.
- Using a soft brush, they'll take a small sample of cells from your cervix.
- The nurse will close and remove the speculum and leave you to get dressed.
Important
You're in control of the screening and can ask the nurse to stop at any time.
Things you can try to make the test easier
If you're worried about cervical screening, there are things you can try that might make the test easier for you:
Do:
- wear something you can leave on during the test, like a skirt or long jumper
- bring someone with you for support
- try breathing exercises to help you relax – ask the nurse about these
- ask the nurse to use a smaller speculum
- ask the nurse about lying in a different position – such as on your side with your knees pulled up to your chest
- bring something to listen to or read during the test
Don't:
- do not feel pressure to keep going – you can ask to stop the test at any time
- try not to be afraid or embarrassed to talk to the nurse – telling them how you feel will help them understand what kinds of support you might need
Things to look out for after cervical screening
You may have some spotting or light bleeding after your cervical screening test.
This is very common and should go away after a few hours.
See a GP if you have:
- heavy bleeding after cervical screening
- any bleeding after cervical screening that does not stop after a few hours
Results
Your cervical screening results are usually sent to you in a letter. Sometimes you may be asked to call your GP to get the results.
When your results should arrive
The nurse or doctor who does your cervical screening test will tell you when you can expect your results letter.
If you have waited longer than you expected, call your GP surgery to see if they have any updates.
Try not to worry if your results are taking a long time to get to you.
It does not mean anything is wrong, and most people will have a normal result.
What your results mean
Your results letter will explain what was tested for and what your results mean.
Sometimes you'll be asked to come back in 3 months to have the test again. This does not mean there's anything wrong – it's because the results were unclear. This is sometimes called an inadequate result.
Human papillomavirus (HPV) is not found in your sample
Most people will not have HPV (an HPV negative result).
This means your risk of getting cervical cancer is very low. You do not need any further tests to check for abnormal cervical cells, even if you have had these in the past.
You'll be invited for screening again in 3 or 5 years.
HPV is found in your sample
Your results letter will explain what will happen next if HPV is found in your sample (an HPV positive result).
You may need:
- another cervical screening test in 1 year
- a different test to look at your cervix (colposcopy)
There are 2 different kinds of HPV positive result:
- HPV found (HPV positive) but no abnormal cells - you'll be invited for screening in 1 year and again in 2 years if you still have HPV. If you still have HPV after 3 years, you may need to have a colposcopy.
- HPV found (HPV positive) and abnormal cells - you'll be asked to have a colposcopy.
HPV is a common virus and most people will get it at some point. You can get it through any kind of sexual contact.
Important
Having a positive HPV result does not mean your partner has had sex with someone else while you have been together.
You might have HPV even if you have not been sexually active or not had a new partner for many years.
If you need a colposcopy
A colposcopy is a simple procedure to look at your cervix.
It's similar to having cervical screening, but it's done in hospital.
You might need a colposcopy if your results show changes to the cells of your cervix.
Find out more about having a colposcopy
Information:
Try not to worry if you have been referred for a colposcopy.
Any changes to your cells will not get worse while you're waiting for your appointment.
The information on this page has been adapted by NHS Wales from original content supplied by  NHS website nhs.uk
NHS website nhs.uk
Last Updated:
06/12/2024 10:48:46