Overview
A hysterectomy is a surgical procedure to remove the womb (uterus). After the operation you will no longer be able to get pregnant.
If you haven't already gone through the menopause, you will also no longer have periods, regardless of your age.
Many women have a hysterectomy. It's more common for women aged 40 to 50.
Why do I need a hysterectomy?
Hysterectomies are carried out to treat health problems that affect the female reproductive system.
These include:
A hysterectomy is a major operation with a long recovery time and is only considered after less invasive treatments have been tried.
Read more about why a hysterectomy is needed.
Things to consider
If you have a hysterectomy, as well as having your womb removed, you may have to decide whether to also have your cervix or ovaries removed.
Your decision will usually be based on your personal feelings, medical history and any recommendations your doctor may have.
Read more information about the things to consider before having a hysterectomy.
Types of hysterectomy
There are various types of hysterectomy. The type you have depends on why you need the operation and how much of your womb and surrounding reproductive system can safely be left in place.
The main types of hysterectomy are:
- total hysterectomy: the womb and cervix (neck of the womb) are removed; this is the most commonly performed operation
- subtotal hysterectomy: the main body of the womb is removed, leaving the cervix in place
- total hysterectomy with bilateral salpingo-oophorectomy: the womb, cervix, fallopian tubes (salpingectomy) and ovaries (oophorectomy) are removed
- radical hysterectomy: the womb and surrounding tissues are removed, including the fallopian tubes, part of the vagina, ovaries, lymph glands and fatty tissue
There are three ways to carry out a hysterectomy:
- vaginal hysterectomy: where the womb is removed through a cut in the top of the vagina
- abdominal hysterectomy: where the womb is removed through a cut in the lower abdomen
- laparoscopic hysterectomy (keyhole surgery): where the womb is removed through several small cuts in the abdomen
Read more about how a hysterectomy is performed.
Complications of a hysterectomy
There is a small risk of complications, including:
- heavy bleeding
- infection
- damage to your bladder or bowel
- serious reaction to the general anaesthetic.
Read more about the complications of a hysterectomy.
Recovering from a hysterectomy
A hysterectomy is a major operation. You can be in hospital for up to five days following surgery, and it takes about six to eight weeks to fully recover.
Recovery times can also vary depending on the type of hysterectomy.
Rest as much as possible during this time and don't lift anything heavy, such as bags of shopping. You need time for your abdominal muscles and tissues to heal.
Read more about recovering from a hysterectomy.
Surgical menopause
If your ovaries are removed during a hysterectomy, you will go through the menopause immediately after the operation, regardless of your age. This is known as a surgical menopause.
If one or both of your ovaries are left intact, there's a chance you will experience the menopause within five years of having your operation.
If you experience a surgical menopause after having a hysterectomy, you should be offered hormone replacement therapy (HRT).
Read more about surgical menopause.
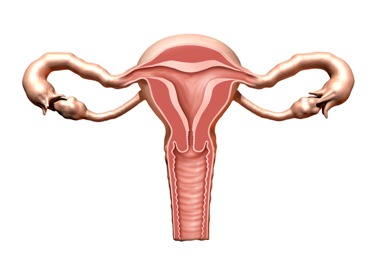
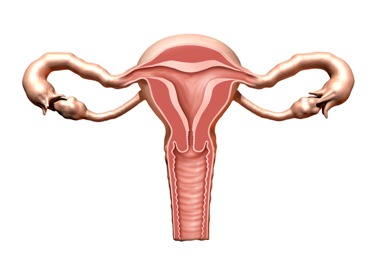
The female reproductive system
The female reproductive system is made up of the:
- womb (uterus) – a pear-shaped organ in the middle of your pelvis where a baby develops; the lining of the womb is shed during a period
- cervix – the neck of the womb, where the womb meets the vagina; the cervix is the lower part of the womb and not separate
- vagina – a muscular tube below the cervix
- fallopian tubes – tubes that connect the womb to the ovaries
- ovaries – small organs by the fallopian tubes that release an egg each month
Why is it necessary?
A hysterectomy is a major operation for a woman that will only be recommended if other treatment options have been unsuccessful.
The most common reasons for having a hysterectomy include:
- heavy periods - which may be caused by fibroids
- pelvic pain - which may be caused by endometriosis, unsuccessfully treated pelvic inflammatory disease (PID) adenomyosis or fibroids
- prolapse of the uterus
- cancer of the womb, ovaries or cervix
Heavy periods
Many women lose a large amount of blood during their periods. They may also experience other symptoms, such as pain and stomach cramps.
For some women, the symptoms can have a significant impact on their quality of life.
Sometimes heavy periods can be caused by fibroids, but in many cases there's no obvious cause.
In some cases, removing the womb may be the only way of stopping persistent heavy menstrual bleeding when:
- other treatments have not worked
- the bleeding has a significant impact on quality of life and it is preferable for periods to stop
- the woman no longer wishes to have children
Read more about heavy periods.
Pelvic inflammatory disease
PID is a bacterial infection of the female reproductive system.
If detected early, the infection can be treated with antibiotics. But if it spreads, it can damage the womb and fallopian tubes, resulting in long-term pain.
A hysterectomy to remove the womb and fallopian tubes may be recommended if a woman has severe pain from PID and no longer wants children.
Read more about pelvic inflammatory disease.
Endometriosis
Endometriosis is where cells that line the womb are also found in other areas of the body and reproductive system, such as the ovaries, fallopian tubes, bladder and rectum.
If the cells that make up the lining of the womb become trapped in other areas of the body, it can cause the surrounding tissue to become inflamed and damaged.
This can lead to pain, heavy and irregular periods, and infertility.
A hysterectomy may remove the areas of endometrial tissue causing the pain.
But it'll usually only be considered if other less invasive treatments have not worked and the woman decides not to have any more children.
Read more about endometriosis.
Fibroids
Fibroids are non-cancerous growths in or around the womb (uterus). The growths are made up of muscle and fibrous tissue, and vary in size.
The symptoms of fibroids can include:
- heavy or painful periods
- pelvic pain
- frequent urination or constipation
- pain or discomfort during sex
A hysterectomy may be recommended if you have large fibroids or severe bleeding and you do not want to have any more children.
Read more about fibroids.
Adenomyosis
Adenomyosis is where the tissue that normally lines the womb starts to grow within the muscular wall of the womb.
This extra tissue can make your periods particularly painful and cause pelvic pain.
A hysterectomy can cure adenomyosis, but will only be considered if all other treatments have failed and you do not want to have any more children.
Prolapse of the uterus
A prolapsed uterus happens when the tissues and ligaments that support the womb become weak, causing it to drop down from its normal position.
Symptoms can include:
A prolapsed uterus can often occur as a result of childbirth.
A hysterectomy resolves the symptoms of a prolapse because it removes the entire womb.
It may be recommended if the tissues and ligaments that support the womb are severely weakened and the woman does not want any more children.
Read more about prolapse of the uterus.
Cancer
A hysterectomy may be recommended for these cancers:
If the cancer has spread and reached an advanced stage, a hysterectomy may be the only viable treatment option.
Deciding to have a hysterectomy
If you have cancer, a hysterectomy may be the only treatment option.
For other health problems, it's a good idea to ask yourself these questions before deciding to have the procedure:
- Are my symptoms seriously affecting my quality of life?
- Have I explored all other treatment options?
- Am I prepared for the possibility of an early menopause?
- Do I still want to have children?
Do not be afraid to ask your doctor as many questions as you want.
Considerations
If you have a hysterectomy, as well as having your womb removed, you may have to decide whether to have your cervix or ovaries removed.
These decisions are usually made based on:
- your medical history
- your doctor's recommendations
- your personal feelings
It's important that you're aware of the different types of hysterectomy and their implications.
Removal of the cervix (total or radical hysterectomy)
If you have cancer of the cervix, ovarian cancer or womb (uterus) cancer, you may be advised to have your cervix removed to stop the cancer spreading.
Even if you do not have cancer, removing the cervix takes away any risk of developing cervical cancer in the future.
Many women are concerned that removing the cervix will lead to a loss in sexual function, but there's no evidence to support this.
Some women are reluctant to have their cervix removed because they want to retain as much of their reproductive system as possible.
If you feel this way, ask your surgeon whether there are any risks associated with keeping your cervix.
If you have your cervix removed, you'll no longer need to have cervical screening tests.
If you do not have your cervix removed, you'll need to continue having regular cervical screening.
Removal of the ovaries (salpingo-oophorectomy)
The National Institute for Health and Care Excellence (NICE) recommends that a woman's ovaries should only be removed if there's a significant risk of associated disease, such as ovarian cancer.
If you have a family history of ovarian or breast cancer, removing your ovaries may be recommended to prevent you getting cancer in the future.
Your surgeon can discuss the pros and cons of removing your ovaries with you. If your ovaries are removed, your fallopian tubes will also be removed.
If you have already gone through the menopause or you're close to it, removing your ovaries may be recommended regardless of the reason for having a hysterectomy.
This is to protect against the possibility of ovarian cancer developing.
Some surgeons feel it's best to leave healthy ovaries in place if the risk of ovarian cancer is small – for example, if there's no family history of the condition.
This is because the ovaries produce several female hormones that can help protect against health problems such as weak bones (osteoporosis). They also play a part in feelings of sexual desire and pleasure.
If you'd prefer to keep your ovaries, make sure you have made this clear to your surgeon before your operation.
You may still be asked to give consent to treatment for having your ovaries removed if an abnormality is found during the operation.
Think carefully about this and discuss any fears or concerns you have with your surgeon.
Surgical menopause
If you have a total or radical hysterectomy that removes your ovaries, you'll experience the menopause immediately after your operation, regardless of your age. This is known as a surgical menopause.
If a hysterectomy leaves 1 or both of your ovaries intact, there's a chance that you'll experience the menopause within 5 years of having the operation.
Although your hormone levels decrease after the menopause, your ovaries continue producing testosterone for up to 20 years.
Testosterone is a hormone that plays an important part in stimulating sexual desire and sexual pleasure.
Your ovaries also continue to produce small amounts of the hormone oestrogen after the menopause.
It's a lack of oestrogen that causes menopausal symptoms such as:
Hormone replacement therapy (HRT) is usually used to help with menopausal symptoms that occur after a hysterectomy.
Hormone replacement therapy (HRT)
You may be offered HRT after having your ovaries removed. This replaces some of the hormones your ovaries used to produce and relieves any menopausal symptoms you may have.
It's unlikely that the HRT you're offered will exactly match the hormones your ovaries previously produced.
The amount of hormones a woman produces can vary greatly, and you may need to try different doses and brands of HRT before you find one that feels suitable.
Not everyone is suitable for HRT. For example, it's not recommended for women who have had a hormone-dependent type of breast cancer or liver disease.
It's important to let your surgeon know about any such health problems you have had.
If you're able to have HRT and both of your ovaries have been removed, it's important to continue with the treatment until you reach the normal age for the menopause (51 is the average age).
Read more about hormone replacement therapy
Cervical screening
If your cervix is removed during a hysterectomy, you'll no longer need to have cervical screening.
If your cervix is left in place after having a subtotal hysterectomy, you'll need to continue to go for regular cervical screening tests.
How is it performed?
There are different types of hysterectomy. The operation you have will depend on the reason for surgery and how much of your womb and reproductive system can safely be left in place.
The main types of hysterectomy are described below.
Total hysterectomy
During a total hysterectomy, your womb and cervix (neck of the womb) is removed.
A total hysterectomy is usually the preferred option over a subtotal hysterectomy, as removing the cervix means there's no risk of you developing cervical cancer at a later date.
Subtotal hysterectomy
A subtotal hysterectomy involves removing the main body of the womb and leaving the cervix in place.
This procedure is not performed very often. If the cervix is left in place, there's still a risk of cervical cancer developing and regular cervical screening will still be needed.
Some women want to keep as much of their reproductive system as possible, including their cervix.
If you feel this way, talk to your surgeon about any risks associated with keeping your cervix.
Total hysterectomy with bilateral salpingo-oophorectomy
A total hysterectomy with bilateral salpingo-oophorectomy is a hysterectomy that also involves removing:
- the fallopian tubes (salpingectomy)
- the ovaries (oophorectomy)
The National Institute for Health and Care Excellence (NICE) recommends that the ovaries should only be removed if there's a significant risk of further problems – for example, if there's a family history of ovarian cancer.
Your surgeon can discuss the pros and cons of removing your ovaries with you.
Radical hysterectomy
A radical hysterectomy is usually carried out to remove and treat cancer when other treatments, such as chemotherapy and radiotherapy, are not suitable or have not worked.
During the procedure, the body of your womb and cervix is removed, along with:
- your fallopian tubes
- part of your vagina
- ovaries
- lymph glands
- fatty tissue
Performing a hysterectomy
There are three ways that a hysterectomy can be performed.
They are:
- vaginal hysterectomy
- abdominal hysterectomy
- laparascopic hysterectomy
Vaginal hysterectomy
During a vaginal hysterectomy, the womb and cervix are removed through an incision that's made in the top of the vagina.
Special surgical instruments are inserted into the vagina to detach the womb from the ligaments that hold it in place.
After the womb and cervix have been removed, the incision will be sewn up. The operation usually takes about an hour to complete.
A vaginal hysterectomy can either be carried out using:
- general anaesthetic – where you'll be unconscious during the procedure
- local anaesthetic – where you'll be awake, but will not feel any pain
- spinal anaesthetic – where you'll be numb from the waist down
A vaginal hysterectomy is usually preferred over an abdominal hysterectomy as it's less invasive and involves a shorter stay in hospital. The recovery time also tends to be quicker.
Abdominal hysterectomy
During an abdominal hysterectomy, an incision will be made in your tummy (abdomen). It'll either be made horizontally along your bikini line, or vertically from your belly button to your bikini line.
A vertical incision will usually be used if there are large fibroids (non-cancerous growths) in your womb, or for some types of cancer.
After your womb has been removed, the incision is stitched up. The operation takes about an hour to perform and a general anaesthetic is used.
An abdominal hysterectomy may be recommended if your womb is enlarged by fibroids or pelvic tumours and it's not possible to remove it through your vagina.
It may also be recommended if your ovaries need to be removed.
Laparoscopic hysterectomy
Laparoscopic surgery is also known as keyhole surgery. It's the preferred way to remove the organs and surrounding tissues of the reproductive system.
During the procedure, a small tube containing a telescope (laparoscope) and a tiny video camera will be inserted through a small cut (incision) in your tummy.
This allows the surgeon to see your internal organs. Instruments are then inserted through other small incisions in your abdomen or vagina to remove your womb, cervix and any other parts of your reproductive system.
Laparoscopic hysterectomies are usually carried out under general anaesthetic.
Getting ready
If you need to have a hysterectomy, it's important to be as fit and healthy as possible.
Good health before your operation will reduce your risk of developing complications and speed up your recovery.
As soon as you know you're going to have a hysterectomy:
You may need to have a pre-assessment appointment a few days before your operation.
This may involve having some blood tests and a general health check to ensure you're fit for surgery.
It's also a good opportunity to discuss any concerns and to ask questions.
Read more about preparing for surgery.
Recovery
After having a hysterectomy, you may wake up feeling tired and in some pain. This is normal after this type of surgery.
You'll be given painkillers to help reduce any pain and discomfort.
If you feel sick after the anaesthetic, your nurse can give you medicine to help relieve this.
You may have:
- dressings placed over your wounds
- a drip in your arm
- a catheter – a small tube that drains urine from your bladder into a collection bag
- a drainage tube in your abdomen (if you've had an abdominal hysterectomy) to take away any blood from beneath your wound – these tubes usually stay in place for one to two days
- a gauze pack inserted into your vagina (if you've had a vaginal hysterectomy) to minimise the risk of bleeding – this usually stays in place for 24 hours
You may also be slightly uncomfortable and feel like you need to poo.
The day after your operation, you'll be encouraged to take a short walk.
This helps your blood to flow normally, reducing the risk of complications developing, such as blood clots in your legs (deep vein thrombosis).
A physiotherapist may show you how to do some exercises to help your mobility.
They may also show you some pelvic floor muscle exercises to help with your recovery.
After the catheter has been removed, you should be able to pass urine normally.
Any stitches that need to be removed will be taken out 5 to 7 days after your operation.
Your recovery time
The length of time it'll take before you're well enough to leave hospital depends on your age and your general level of health.
If you have had a vaginal or laparoscopic hysterectomy, you may be able to leave between 1 and 4 days later.
If you have had an abdominal hysterectomy, it'll usually be up to 5 days before you're discharged.
You may be asked to see your GP in 4 to 6 weeks, but follow-up appointments with the hospital are not usually needed unless there are complications.
It takes about 6 to 8 weeks to fully recover after having an abdominal hysterectomy.
Recovery times are often shorter after a vaginal or laparoscopy hysterectomy.
During this time, you should rest as much as possible and not lift anything heavy, such as bags of shopping.
Your abdominal muscles and the surrounding tissues need time to heal.
If you live by yourself, you may be able to get help while you're recovering from your operation.
Hospital staff should be able to advise you further about this.
Side effects
After having a hysterectomy, you may have some temporary side effects.
Bowel and bladder disturbances
After your operation, there may be some changes in your bowel and bladder functions when going to the toilet.
Some women develop urinary tract infections or constipation. Both can easily be treated.
It's recommended that you drink plenty of fluids and increase the fruit and fibre in your diet to help with your bowel and bladder movements.
For the first few bowel movements after a hysterectomy, you may need laxatives to help you avoid straining.
Some people find it more comfortable to hold their abdomen to provide support while passing a stool.
Vaginal discharge
After a hysterectomy, you'll experience some vaginal bleeding and discharge.
This will be less discharge than during a period, but it may last up to 6 weeks.
Visit your GP if you experience heavy vaginal bleeding, start passing blood clots or have a strong-smelling discharge.
Menopausal symptoms
If your ovaries are removed, you'll usually experience severe menopausal symptoms after your operation.
These may include:
- hot flushes
- anxiety
- weepiness
- sweating
You may have hormone replacement therapy (HRT) after your operation.
This can be given in the form of an implant, injections or tablets.
It usually takes around a week before having an effect.
Emotional effects
You may feel a sense of loss and sadness after having a hysterectomy.
These feelings are particularly common in women with advanced cancer, who have no other treatment option.
Some women who have not yet experienced the menopause may feel a sense of loss because they're no longer able to have children. Others may feel less "womanly" than before.
In some cases, having a hysterectomy can be a trigger for depression.
See your GP if you have feelings of depression that will not go away, as they can advise you about the available treatment options.
Talking to other women who have had a hysterectomy may help by providing emotional support and reassurance.
Your GP or the hospital staff may be able to recommend a local support group.
Getting back to normal
Returning to work
How long it'll take for you to return to work depends on how you feel and what sort of work you do.
If your job does not involve manual work or heavy lifting, it may be possible to return after 4 to 8 weeks.
Driving
Do not drive until you're comfortable wearing a seatbelt and can safely perform an emergency stop.
This can be anything from 3 to 8 weeks after your operation.
You may want to check with your GP that you're fit to drive before you start.
Some car insurance companies require a certificate from a GP stating that you're fit to drive. Check this with your car insurance company.
Exercise and lifting
After a hysterectomy, the hospital where you were treated should give you information and advice about suitable forms of exercise while you recover.
Walking is always recommended, and you can swim after your wounds have healed.
Do not try to do too much as you'll probably feel more tired than usual.
Do not lift any heavy objects during your recovery period.
If you have to lift light objects, make sure your knees are bent and your back is straight.
Sex
After a hysterectomy, it's generally recommended that you do not have sex until your scars have healed and any vaginal discharge has stopped, which usually takes at least 4 to 6 weeks.
As long as you're comfortable and relaxed, it's safe to have sex.
You may experience some vaginal dryness, particularly if you have had your ovaries removed and you're not taking HRT.
Many women also experience an initial loss of sexual desire (libido) after the operation, but this usually returns once they have fully recovered.
At this point, studies show that pain during sex is reduced and strength of orgasm, libido and sexual activity all improve after a hysterectomy.
Contraception
You no longer need to use contraception to prevent pregnancy after having a hysterectomy.
But you'll still need to use condoms to protect yourself against sexually transmitted infections (STIs).
Complications
As with all types of surgery, a hysterectomy can sometimes lead to complications.
Some of the possible complications are:
- general anaesthetic complications
- bleeding
- ureter damage
- bladder or bowel damage
- infection
- blood clots
- vaginal problems
- ovary failure
- early menopause
General anaesthetic
It's very rare for serious complications to happen after having a general anaesthetic.
Serious complications can include nerve damage, allergic reaction and death. But death is very rare.
Being fit and healthy before you have an operation reduces your risk of developing complications.
Bleeding
As with all major operations, there's a small risk of heavy bleeding (haemorrhage) after having a hysterectomy.
If you have heavy bleeding, you may need a blood transfusion.
Ureter damage
The ureter (the tube that urine is passed through) may be damaged during surgery.
This is a rare complication and it's usually repaired during the hysterectomy.
Bladder or bowel damage
In rare cases, there's damage to abdominal organs such as the bladder or bowel.
This can cause problems such as:
- infection
- incontinence
- needing to pee often
It may be possible to repair any damage during the hysterectomy. You may need a temporary catheter to drain your urine or a colostomy to collect your bowel movements.
Infection
There's always a risk of an infection after an operation. This could be a wound infection or a urinary tract infection.
These are not usually serious and can be treated with antibiotics.
Blood clots
A blood clot, also known as a thrombosis, can form in a vein and interferes with blood circulation and the flow of oxygen around the body.
The risk of getting blood clots increases after having operations and periods of immobility.
You'll be encouraged to start moving around as soon as possible after your operation.
You may also be given an injection of a blood-thinning medication (anticoagulant) to reduce the risk of clots.
Vaginal problems
If you have a vaginal hysterectomy, there's a risk of problems at the top of your vagina where the cervix was removed.
This could range from infection or slow wound healing after the operation to prolapse in later years.
Ovary failure
Even if 1 or both of your ovaries are left intact, you may still have symptoms of the menopause earlier than expected.
Early menopause
If you have had your ovaries removed, you'll usually have menopausal symptoms soon after the operation, such as:
- hot flushes
- sweating
- vaginal dryness
- disturbed sleep
This is because your ovaries are no longer releasing the hormone oestrogen and releasing eggs (ovulating).
This is an important consideration if you're under the age of 40, as early onset of the menopause can increase your risk of developing weak bones (osteoporosis).
This is because oestrogen levels decrease during the menopause.
Depending on your age and circumstances, you may need to take extra medicine to prevent osteoporosis.
The information on this page has been adapted by NHS Wales from original content supplied by  NHS website nhs.uk
NHS website nhs.uk
Last Updated:
06/10/2023 15:37:37