Overview
Sickle cell disorder is the name for a group of inherited health conditions that affect the red blood cells. The most serious type is called sickle cell anaemia.
Sickle cell disorder is particularly common in people with an African or Caribbean family background.
People with sickle cell disorder produce unusually shaped red blood cells that can cause problems because they do not live as long as healthy blood cells and can block blood vessels.
Sickle cell disorder is a serious and lifelong health condition, although treatment can help manage many of the symptoms.
Symptoms of sickle cell disorder
People born with sickle cell disorder sometimes tend to have problems from early childhood, although some children have few symptoms and lead normal lives most of the time.
The main symptoms of sickle cell disorder are:
- painful episodes called sickle cell crises, which can be very severe and can last up to a week
- an increased risk of serious infections
- anaemia (where red blood cells can't carry enough oxygen around the body), which can cause tiredness and shortness of breath
Some people also experience other problems such as delayed growth, strokes and lung problems.
Causes of sickle cell disorder
Sickle cell disorder is caused by a gene that affects how red blood cells develop.
If both parents have the gene, there's a 1 in 4 chance of each child they have being born with sickle cell disorder.
The child's parents often won't have the condition themselves because they're only carriers of the sickle cell trait.
Screening and testing for sickle cell disorder
Sickle cell disorder is often detected during pregnancy or soon after birth.
Screening for sickle cell disorder in pregnancy is offered to all pregnant women in Wales to check if there's a risk of a child being born with the condition, and all babies are offered screening as part of the newborn bloodspot screening test (heel prick test).
Blood tests can also be carried out at any age to check for sickle cell disease to see if you're a carrier of the gene that causes it.
Treatments for sickle cell disorder
People with sickle cell disorder need treatment throughout their lives. This is usually delivered by different health professionals in a specialist sickle cell centre.
It's also important for people with sickle cell disorder to look after their own health using self care measures, such as by avoiding triggers and managing pain.
A number of treatments for sickle cell disorder are available.
For example:
- drinking plenty of fluids and staying warm to prevent painful episodes
- painkillers, such as paracetamol or ibuprofen (sometimes treatment with stronger painkillers in hospital may be necessary)
- daily antibiotics and having regular vaccinations to reduce your chances of getting an infection
- a medicine called hydroxycarbamide (hydroxyurea) and crizanlizumab to reduce symptoms
- regular blood transfusions if symptoms continue or get worse, or there are signs of damage caused by sickle cell disease
- an emergency blood transfusion if severe anaemia develops
The only cure for sickle cell disorder is a stem cell or bone marrow transplant, but they're not done very often because of the risks involved.
Outlook for sickle cell disorder
Sickle cell disorder varies between individuals from mild to serious, but most people with it lead happy and normal lives.
Mild sickle cell disorder may have no impact on a person's day-to-day life.
But the illness can be serious enough to have a significant effect on a person's life.
It can lead to health problems like strokes, serious infections and lung problems, which can occasionally be fatal.
Overall, the life expectancy for someone with sickle cell disorder tends to be shorter than normal, but this can vary depending on the exact type of sickle cell disease they have, how it's treated and what problems they experience.
Carriers of sickle cell (sickle cell trait)
A carrier of sickle cell is someone who carries the gene that causes sickle cell disorder, but does not have the condition themselves. It's also known as having the sickle cell trait.
People who carry sickle cell will not develop sickle cell disorder, but are at risk of having a child with it if their partner is also a carrier.
You can request a blood test to check if you carry the sickle cell trait from your GP surgery or the nearest sickle cell thalassaemia centre.
More information and support
Finding out as much as possible about sickle cell disorder may help you feel more in control of your illness.
The Sickle Cell Society is a UK charity for people with sickle cell disease.
Their website has a wide range of useful information, including news about research into the disorder and details of suport groups.
Symptoms
Sickle cell disorder can cause a wide range of symptoms.
These can start from a few months of age, although many children have few or no symptoms if treatment is started early on.
The main symptoms are:
- painful episodes
- getting infections often
- anaemia
Painful episodes
Episodes of pain known as sickle cell crises are one of the most common and distressing symptoms of sickle cell disorder.
They happen when blood vessels to part of the body become blocked.
The pain can be severe and lasts for several days or weeks.
A sickle cell crisis can affect any part of the body, but is most common in the limbs or back:
How often someone with sickle cell disorder gets episodes of pain varies a lot.
Some people may have one every week, while others may have less than 1 a year.
It's not always clear what triggers bad pain, but sometimes painful episodes can be caused by the weather (such as wind, rain or cold), dehydration, stress or strenuous exercise.
Infections
People with sickle cell disorder are more vulnerable to infections, particularly when they're young.
Infections can range from mild, such as colds, to much more serious and potentially life threatening, such as meningitis.
Vaccinations and daily doses of antibiotics can help reduce the risk of many infections.
Anaemia
Nearly all people with sickle cell disorder have anaemia, where the haemoglobin in the blood is low.
Haemoglobin is the substance found in red blood cells that's used to transport oxygen around the body.
This does not usually cause many symptoms, but sometimes it can get worse if you become infected with the virus that causes slapped cheek syndrome (parvovirus).
This can lead to a sudden drop in the number of red blood cells and may cause additional symptoms such as headaches, a rapid heartbeat, dizziness and fainting.
It's usually treated with a blood transfusion.
Other problems
Sickle cell disorder can also sometimes cause a wide range of other problems.
These include:
- delayed growth during childhood and delayed puberty
- gallstones (small stones in the gallbladder), which can cause tummy (abdominal) pain and yellow skin and eyes (jaundice)
- bone and joint pain
- priapism (a persistent and painful erection of the penis), which can sometimes last several hours
- leg ulcers (painful, open sores on the lower legs)
- strokes or transient ischaemic attacks (where the flow of blood to the brain is blocked or interrupted)
- a serious lung condition called acute chest syndrome, which can cause a fever, cough, chest pain, and breathing difficulties
- swelling of the spleen, which can cause shortness of breath, a rapid heartbeat, tummy pain, a swollen tummy and anaemia
- eyesight problems, such as floaters, blurred or patchy vision, reduced night vision and occasionally sudden vision loss
- pulmonary hypertension (high blood pressure in the blood vessels that carry blood from the heart to the lungs)
- kidney or urinary problems, including blood in the urine and bedwetting
Who can get it
Sickle cell disorder is caused by inheriting the sickle cell gene.
It's not caused by anything the parents did before or during the pregnancy and you cannot catch it from someone who has it.
How sickle cell disorder is inherited
Genes come in pairs. You inherit 1 set from your mother and 1 set from your father.
To be born with sickle cell disease, a child has to inherit a copy of the sickle cell gene from both of their parents.
This usually happens when both parents are "carriers" of the sickle cell gene, also known as having the sickle cell trait.
Or it can happen when 1 parent has sickle cell disorder and the other is a carrier of it.
Sickle cell carriers do not have sickle cell disorder themselves, but there's a chance they could have a child with the condition if their partner is also a carrier.
If both parents are sickle cell carriers, there's a:
- 1 in 4 chance each child they have will not inherit any sickle cell genes and will not have sickle cell disease or be able to pass it on
- 1 in 2 chance each child they have will just inherit a copy of the sickle cell gene from 1 parent and be a carrier
- 1 in 4 chance each child they have will inherit copies of the sickle cell gene from both parents and will be born with sickle cell disease
The Sickle Cell Society has more information about the inheritance of sickle cell disease, including what the risks are if a parent has sickle cell disorder themselves.
Who's most at risk of sickle cell disorder?
In the UK, sickle cell disorder is most commonly seen in people of African and Caribbean backgrounds.
A simple blood test will show whether you're a carrier. This is done routinely during pregnancy and after birth, but you can ask to have the test at any time.
How sickle cell disorder affects the body
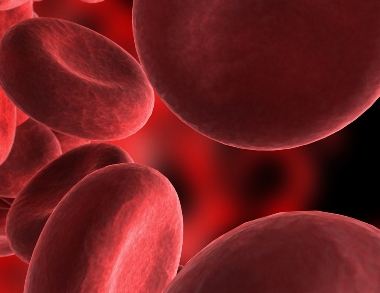
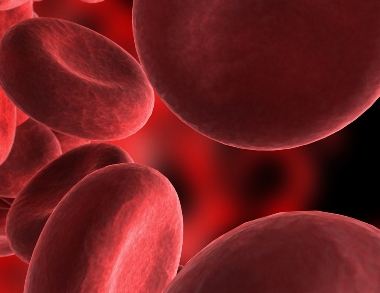
Your genes are the set of instructions found inside every cell in your body. They determine characteristics like the colour of your eyes and hair.
People with sickle cell disorder do not make haemoglobin properly. Haemoglobin is a substance in red blood cells, which carry oxygen around the body.
Normal red blood cells are flexible and disc-shaped, but in sickle cell disease they can become rigid and shaped like a crescent or sickle because the haemoglobin inside them clumps together.
These unusual cells can cause symptoms of sickle cell disorder because they do not live as long as normal red blood cells and can become stuck in blood vessels.
Diagnosis
Sickle cell disorder is usually detected during pregnancy or soon after birth.
Blood tests can also be carried out at any time to check for the condition or to see if you're a sickle cell carrier and are at risk of having a child with the condition.
Sickle cell screening during pregnancy
Screening to check if a baby's at risk of being born with sickle cell disorder is offered to all pregnant women in Wales.
In parts of Wales where sickle cell disorder is more common, pregnant women are offered a blood test to check if they carry sickle cell.
In areas where sickle cell disorder is less common, a questionnaire about your family origins is used to work out whether you should have a blood test for sickle cell.
You can also ask to have the blood test even if your family origins do not suggest your baby would be at high risk of sickle cell disorder.
Screening should ideally be carried out before you're 10 weeks pregnant so you and your partner have time to consider the option of further tests to find out if your baby will be born with sickle cell disorder.
Newborn bloodspot screening for sickle cell disorder
In Wales screening for sickle cell disorder is offered as part of the newborn blood spot test (heel prick test).
This can help to:
- indicate whether your baby has sickle cell disorder if pregnancy screening suggested they were at high risk but you decided not to have tests to confirm the diagnosis at the time
- identify any babies with sickle cell disorder whose parents were not screened during pregnancy
- show if your baby has the sickle cell trait
- pick up certain other inherited conditions, such as cystic fibrosis
If newborn screening suggests your baby may have sickle cell disorder, a second blood test will be carried out to confirm the diagnosis.
Testing for the sickle cell carriers
A blood test can be done at any time to find out if you carry sickle cell and are at risk of having a child with sickle cell disorder.
This is also known as having the sickle cell trait.
Getting tested can be particularly useful if you have a family history of sickle cell disease or your partner is known to carry the sickle cell trait.
If you think you could be a carrier, talk to a GP about having the test.
Both men and women can have the test.
Treatment
Sickle cell disorder usually requires lifelong treatment.
Children and adults with sickle cell disease will be supported by a team of different healthcare professionals working together at a specialist sickle cell centre.
Your healthcare team will help you learn more about sickle cell disorder, and work with you to come up with an individual care plan that takes into account all your needs and health concerns.
Preventing painful episodes
The main thing you can do to reduce your chances of experiencing a painful episode (sickle cell crisis) is to try avoiding possible triggers.
This may mean you need to:
- drink plenty of fluids to avoid dehydration
- wear appropriate clothing to stop you getting cold
- avoid sudden temperature changes, such as swimming in cold water
Medicine for sickle cell pain
If you continue to have episodes of pain, a medicine called hydroxycarbamide (hydroxyurea) may be recommended. You usually take it as a capsule once a day.
Hydroxycarbamide can lower the amount of other blood cells, such as white blood cells and platelets (clotting cells), so you'll usually have regular blood tests to monitor your health.
If you have regular episodes of pain, you may also be able to have a medicine called crizanlizumab. Crizanlizumab can be taken on its own or alongside hydroxycarbamide. You will usually be given crizanlizumab by injection into a vein every 4 weeks.
Find out more about crizanlizumab from the National Institute for Health and Care Excellence (NICE).
Self-help for treating a sickle cell crisis
If you have a sickle cell crisis, you can usually manage it at home.
The following things can help:
- take over-the-counter painkillers, such as paracetamol or ibuprofen (do not give aspirin to children under 16 unless a doctor has prescribed it) – if the pain is more severe, your GP may prescribe stronger painkillers
- have plenty to drink
- use a warm towel or a wrapped heated pad to gently massage the affected body part – many pharmacies sell heat pads that you can use for this purpose
- distractions to take your mind off the pain – for example, children might like to read a story, watch a film or play their favourite computer game
Contact your GP if these measures do not work or the pain is particularly severe. If this is not possible, go to your local A&E.
You may need treatment with very strong painkillers, such as morphine, in hospital for a few days.
Preventing infections if you have sickle cell disorder
People with sickle cell disorder are more vulnerable to infections.
Most people need to take a daily dose of antibiotics, usually penicillin, often for the rest of their life.
Long-term use of antibiotics will not pose any serious risks to your health.
Children with sickle cell disorder should also have all the routine vaccinations, and possibly also additional vaccinations like the annual flu vaccine and the hepatitis B vaccine.
Treatments for sickle cell-related anaemia
Anaemia often causes few symptoms and may not require specific treatment.
But dietary supplements like folic acid, which helps stimulate the production of red blood cells, may sometimes be required to help improve anaemia if your child has a restricted diet, such as a vegetarian or vegan diet.
Anaemia caused by sickle cell disorder is not the same as the more common iron deficiency anaemia.
Do not take iron supplements to treat it without seeking medical advice, as they could be dangerous.
If anaemia is particularly severe or persistent, treatment with blood transfusions or hydroxycarbamide may be necessary.
Stem cell or bone marrow transplants
Stem cell or bone marrow transplants are the only cure for sickle cell disorder, but they're not done very often because of the significant risks involved.
Stem cells are special cells produced by bone marrow, a spongy tissue found in the centre of some bones. They can turn into different types of blood cells.
For a stem cell transplant, stem cells from a healthy donor are given through a drip into a vein.
These cells then start to produce healthy red blood cells to replace the sickle cells.
A stem cell transplant is an intensive treatment that carries a number of risks.
The main risk is graft versus host disease, a life-threatening problem where the transplanted cells start to attack the other cells in your body.
Stem cell transplants are generally only considered in children with sickle cell disease who have severe symptoms that have not responded to other treatments, when the long-term benefits of a transplant are thought to outweigh the possible risks.
Treating other problems
Sickle cell disorder can also cause a number of other problems that may need to be treated.
For example:
- a short course of hormonal medicine may be prescribed to trigger puberty in children with delayed puberty
- gallstones may be treated with gallbladder removal surgery
- bone and joint pain can be treated with painkillers, although more severe cases may require surgery
- persistent and painful erections (priapism) may require medication to stimulate blood flow or using a needle to drain blood from the penis
- leg ulcers can be treated by cleaning the ulcer and dressing it with a bandage
- people at increased risk of having a stroke, or those who have had a stroke, may need regular blood transfusions or treatment with hydroxycarbamide
- acute chest syndrome, a serious lung condition, usually requires emergency treatment with antibiotics, blood transfusions, oxygen and fluids given into a vein – hydroxycarbamide may be needed to prevent further episodes
People who need a lot of blood transfusions may also need to take medicine called chelation therapy. This reduces the amount of iron in their blood to safe levels.
Living with
There are a number of things you can do, and precautions you can take, to stay as healthy as possible if you have sickle cell disorder.
Managing pain
You can reduce your risk of experiencing painful episodes (sickle cell crises) by avoiding things that can trigger them.
Try to:
- drink plenty of fluids, particularly during hot weather – dehydration increases the risk of a sickle cell crisis
- avoid extreme temperatures – you should dress appropriately for the weather and avoid sudden temperature changes such as swimming in cold water
- be careful at high altitudes – the lack of oxygen at high altitudes may trigger a crisis (travelling by plane shouldn't be a problem because planes are pressurised to maintain a steady oxygen level)
- avoid very strenuous exercise – people with sickle cell disease should be active, but intense activities that cause you to become seriously out of breath are best avoided
- avoid alcohol and smoking – alcohol can cause you to become dehydrated and smoking can trigger a serious lung condition called acute chest syndrome
- relax – stress can trigger a sickle cell crisis, so it may help to learn relaxation techniques such as breathing exercises
Your healthcare team can give you more advice about avoiding triggers.
It's also a good idea to ensure you're prepared to treat pain at home. Keep a ready supply of painkillers (paracetamol or ibuprofen) and consider buying some heated pads to soothe the pain.
Avoiding infections
You'll usually be given antibiotics and advised to have vaccinations to help prevent most serious infections, but there are also things you can do to reduce your risk.
For example, you should make sure you follow good food hygiene measures to prevent food poisoning.
Make sure you speak to your GP or healthcare team if you're planning on travelling aboard, as this may mean you need extra medication or vaccinations.
For example, if you're travelling to an area where malaria is found, it's important to take antimalarial medication.
You may also need to take extra food and water precautions abroad.
Pregnancy and contraception
Women with sickle cell disease can have a healthy pregnancy, but it's a good idea to speak to your healthcare team for advice first.
It may be useful to find out if your partner is a carrier of sickle cell and discuss the implications of this with a counsellor.
Some sickle cell disorder medicines, such as hydroxycarbamide, can harm an unborn baby. You may need to be stop taking them before trying to get pregnant.
There's an increased risk of problems, such as anaemia, sickle cell pain, miscarriage and pre-eclampsia, during pregnancy.
And you may need extra monitoring and treatment during pregnancy to help prevent problems.
If you're not planning a pregnancy, use a reliable form of contraception.
Surgery precautions if you have sickle cell disorder
It's important to let your healthcare team know if you need to have an operation under general anaesthetic at any point. Tell your surgeon that you have sickle cell disorder.
This is because general anaesthetic can cause problems for people with sickle cell disease, including an increased risk of experiencing a sickle cell crisis.
You may need close monitoring during surgery to ensure you're getting enough fluids and oxygen and are kept warm.
Sometimes you may be need a blood transfusion beforehand to reduce the risk of complications.
When to get medical advice
Make sure you know when to get medical advice and where to go, as sickle cell disease can cause a number of serious problems that can appear suddenly.
Problems to look out for include:
- a high temperature over 38C (or any increased temperature in a child)
- severe pain that's not responding to treatment at home
- severe vomiting or diarrhoea
- a very severe headache, dizziness or stiff neck
- breathing difficulties
- very pale skin or lips
- sudden swelling in the tummy
- a painful erection (priapism) lasting more than 2 hours
- confusion, drowsiness or slurred speech
- seizures (fits)
- weakness on 1 or both sides of the body
- changes in vision or sudden vision loss
Contact your GP or healthcare team straight away if you develop any of these symptoms.
If this is not possible, go to your nearest A&E. If you're not well enough to travel to hospital yourself, dial 999 for an ambulance.
Make sure that the medical staff looking after you know you have sickle cell disorder.
Carriers
If you're a carrier of sickle cell it means you carry 1 of the genes that causes sickle cell disease, but you do not have the condition yourself.
It's also known as having the sickle cell trait.
People who carry sickle cell won't develop sickle cell disease, but may be at risk of having a child with the condition and may occasionally need to take precautions to stop them becoming unwell.
You can find out if you're a carrier of sickle cell by having a simple blood test.
GOV.UK has a detailed leaflet about being a sickle cell carrier
Who can be a sickle cell carrier?
Anyone can be a carrier of sickle cell, but it's much more common in people from certain ethnic backgrounds.
In the UK, most people who carry the sickle cell trait have an African or Caribbean family background.
Testing for the sickle cell carriers
Screening for sickle cell disease is offered to all pregnant women in Wales, although most women will be at low risk and will not need to have a blood test to check if they're a carrier.
Anyone can ask to have a free blood test to find out if they're a carrier at any point. This can be useful if:
- you want to find out if you're at risk of having a child with sickle cell disease
- you have a family history of sickle cell disease or carrying the sickle cell trait
- your partner carries the sickle cell trait
You can request the test from your GP surgery or nearest genetic counsellor who will discuss the result and implications with you if you're found to carry sickle cell.
Having children
If you carry sickle cell, you're at risk of having children with sickle cell disorder, although this can only happen if the father of your baby is also a carrier or has sickle cell disorder themselves.
If you're planning to have a child and you know you're a carrier, it's a good idea for your partner to be tested.
If you and your partner both carry sickle cell, there's a:
- 1 in 4 chance each child you have will not have sickle cell disorder or be a carrier
- 1 in 2 chance each child you have will be a carrier but will not have sickle cell disorder
- 1 in 4 chance each child you have will be born with sickle cell disorder
If both of you are carriers and you're planning to have a baby, talk to your GP about getting a referral to a genetic counsellor who can explain the risks to your children and what your options are.
These include:
- having tests during pregnancy to see if your baby will have sickle cell disease
- adopting a child
- trying IVF with a donor egg or sperm
- trying pre-implantation genetic diagnosis (PGD)
PGD is similar to IVF, but the resulting embryos are tested to check that they do not have sickle cell disorder before they're implanted in the womb.
Rare health risks
You're not at risk of developing sickle cell disorder if you carry sickle cell.
The only time you may be at risk of health problems is in rare cases where you might not get enough oxygen, such as:
- having surgery under general anaesthetic – make sure medical staff are aware you carry the sickle cell trait before your operation
- during regular intensive physical activity – make sure you drink plenty of fluids during training and avoid extreme exhaustion
There's also a very small risk of developing kidney problems associated with carrying sickle cell.
Apart from these uncommon situations, you can lead a completely normal and healthy life if you're a sickle cell carrier.
People who carry other blood disorders
People who are carriers of sickle cell are also at risk of having a child with a blood disorder if the father of the baby is a carrier of a different type of blood disorder.
You can find more detailed information about some of the other types of carrier in the following leaflets:
The information on this page has been adapted by NHS Wales from original content supplied by  NHS website nhs.uk
NHS website nhs.uk
Last Updated:
21/10/2025 11:22:25